Pancreatic cancer
- davorkust

- Jun 30, 2025
- 5 min read
Updated: Jul 25, 2025
Introduction and incidence
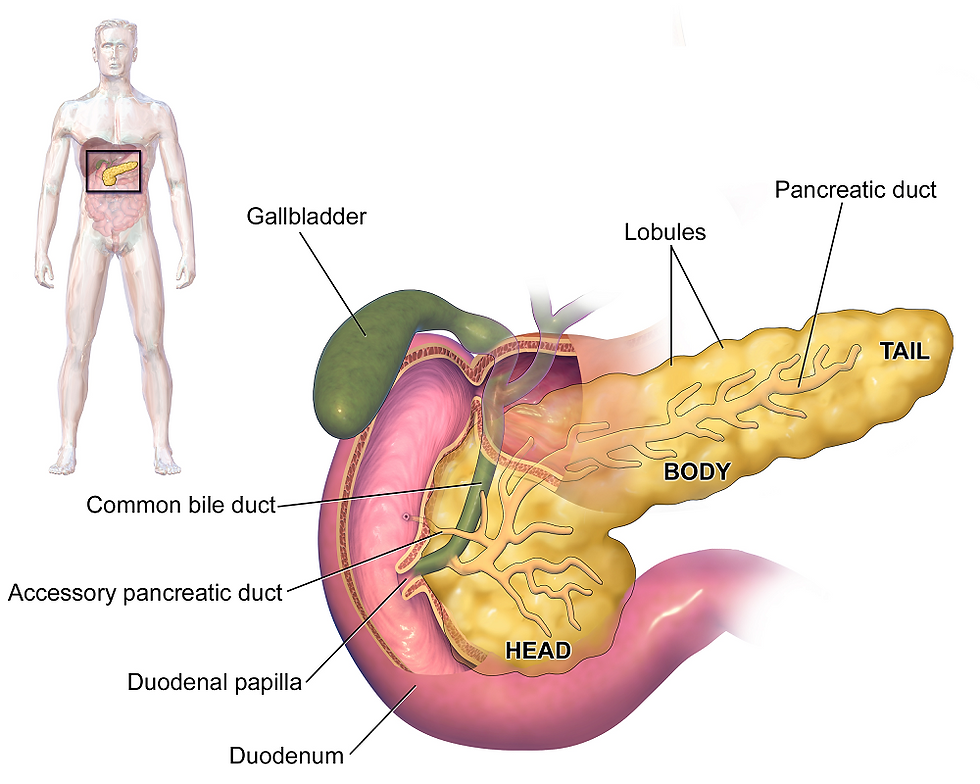
The pancreas is a gland shaped like a horizontally placed thin pear, located between the stomach, small intestine and spine. It consists of 3 parts. The wide part is called the head, which continues into the body and then into a narrower part called the tail (Figure 1). Tumors most often arise in the head area. The pancreas has a dual function: exocrine (it produces enzymes that it secretes into the intestine, which help break down food) and endocrine (it secretes hormones such as insulin and glucagon, which are important in controlling blood sugar levels). About 95% of pancreatic cancer cases arise in exocrine cells (adenocarcinoma), but neuroendocrine tumors that arise from endocrine cells can also develop in the pancreas (more about this disease in a separate article). Pancreatic adenocarcinoma is one of the most aggressive malignant tumors.
Risk factors
Some of the factors that increase the risk of developing pancreatic cancer are smoking, obesity, a positive personal and/or family history of diabetes or chronic pancreatitis, and various genetic syndromes (such as MEN1, Lynch, VHL, and others). In relation to diabetes, it is not only a risk factor but can also be the first early sign of developing pancreatic cancer. Therefore, it is definitely advisable to analyze the pancreatic area in people who suddenly develop diabetes in adulthood. You can read more about the risk factors for cancer in a separate article.
Signs and symptoms
In the early stages of the disease, there are often no noticeable symptoms. As the disease progresses, jaundice (yellowing of the skin and eyes), pale stools, dark urine, pain in the middle-upper abdomen and back (the pain often spreads in a belt-like manner), weight loss for no apparent reason, loss of appetite, and constant fatigue may occur.
Diagnosis
One of the reasons for the high mortality rate of this disease is the late diagnosis due to the absence of early symptoms of the disease. The basis is a detailed examination of the patient and taking a thorough medical history. The initial diagnostic examination is blood tests, with particular attention to bilirubin levels (tumors of the pancreatic head can obstruct the bile ducts and lead to elevated bilirubin levels), and to tumor markers CA19-9 and CEA. Imaging tests include ultrasound, CT, MRI or PET/CT (most often CT). These tests analyze the pancreas area, as well as surrounding organs, for the presence of possible metastases. In the case of findings that indicate the possibility of a pancreatic tumor, there are several ways to obtain a tissue sample for final confirmation of the disease. One of the most commonly used techniques is the use of endoscopic ultrasound (EUS), during which an endoscope inserted through the mouth is brought into close proximity to the pancreas and a tissue sample can be taken. A similar test is the so-called endoscopic retrograde cholangiopancreatography (ERCP), which inserts a catheter (thin tube) into the small pancreatic ducts and, in the event of a tumor blocking the ducts, a stent can be placed in the same procedure. This can help resolve jaundice in patients with obstruction. You can read more about diagnosing malignant diseases in general in a separate article.
Stage of the disease
The prognosis of patients with pancreatic cancer depends on several factors, such as whether the tumor is operable, the stage of the disease, the general condition of the patient, and whether it is the first occurrence of the disease or if the disease has returned after previous treatment. Generally speaking, it is an aggressive disease and it is important to detect the disease as early as possible in order to improve the chances of cure.
In stage I, the disease is limited to the pancreas and the tumor is 4 cm in diameter at most. In stage II, the tumor is larger than 4 cm or lymph nodes are involved (up to 3 nodes at most). In stage III, 4 or more lymph nodes are affected, or large blood vessels around the pancreas are affected. At this stage, complete surgical removal of the disease is usually not possible. Stage IV of the disease indicates the presence of distant metastases.
Treatment
In patients with resectable disease, i.e. in a situation where, according to the tests performed, the tumor mass can be completely removed, the treatment of choice is surgery. The type of surgical treatment depends on the location of the tumor within the pancreas, so for example, in tumors located in the head, the so-called Whipple operation is used (the adjacent part of the small intestine is removed along with the head of the pancreas), and in tumors in the tail, distal pancreatectomy (removal of the tail). Sometimes it is necessary to remove the entire pancreas due to the advanced nature of the disease. After the procedure itself, most patients will be candidates for adjuvant chemotherapy to reduce the risk of the disease returning, and treatment should begin within 12 weeks of surgery. If, on the other hand, the disease is not operable or a unanimous conclusion cannot be reached (so-called borderline resectable disease), treatment can be started with neoadjuvant chemotherapy with the aim of reducing the tumor mass. If the disease responds well to this type of treatment, it will be possible to remove the tumor with surgery in the future. For patients with stage IV disease, surgery is not used. The choice of treatment is one of the systemic therapy options. The above usually includes various chemotherapy protocols, but in patients with detected certain genetic mutations of the tumor tissue, immunotherapy or targeted therapy can be applied. Inclusion in clinical trials with innovative drugs is also an option. Regardless of the choice of therapy, continuous monitoring by the competent oncologist is important, so that the proposed therapy is adequately implemented and the patient's quality of life is preserved.
Treatment at onkologija.net: We treat our patients according to American and Western European guidelines, and we additionally enable genetic testing for the application of personalized targeted therapy. Contact us for more details.
Continue reading:
Potrebno Vam je više informacija o ovoj temi? Kontaktirajte nas.


